Case studies
Utilising AKI alerts to assist in identifying patients who require more specialist support at University Hospital Southampton
Share this on – Facebook / Twitter / Linked In

University Hospital Southampton NHS Foundation Trust is utilising AKI alerts to assist in identifying patients who require more specialist support.
This case study is written by an AKI clinical nurse specialist, Becky Bonfield.
A number of staff receive daily emails with a list of the patients who have AKI.
These include the AKI team (lead consultant and AKI nurse) and pharmacists across the hospital.
As the AKI Clinical Nurse Specialist, I receive a separate list of all the patients across the trust that have stage three AKI, as well as a list with all patients with AKI across the trust. I then review all patients with an AKI stage three outside of critical care areas and patients who are high risk with AKI stage two – these are patients who are in areas which are not experienced in caring for patients with AKI, areas where there is limited access to medical practitioners or patients who have progressing AKI.
For this case study I will use a case review of a patient that the alert system highlighted to me and was subsequently reviewed. The patient will remain anonymous and will be called Mrs Smith.
Mrs Smith had been admitted with pre-eclampsia and had delivered her baby successfully; she had been admitted for several days prior to giving birth for treatment for her condition and had required an emergency caesarean section at 39 weeks gestation.
Post delivery her bloods indicated that she had AKI stage two and she had been reviewed by a pharmacist who had checked her medications to ensure that she wasn’t on any drugs that might cause problems for her kidneys.
The patient was hypertensive, requiring IV nitrate infusion and was being cared for in labour high dependency. I reviewed the patient, taking her history and a physical assessment.
Mrs Smith was normotensive and her IV nitrates were being weaned. I recommended further weaning of her nitrate infusion to optimise her blood pressure, strict fluid balance monitoring, a urinalysis and amending her analgesia as she was prescribed opiates.
Despite these interventions the following day the patient had AKI stage three. I undertook a repeat review alongside the obstetrics team. Mrs Smith’s urinalysis was positive for protein and blood in large quantities. She was passing good volumes of urine but it was very dilute. We requested a urinary PCR and at this point I felt it was appropriate to refer the patient to the renal team for their advice and support.
A joint review with the renal consultant was carried out and a treatment plan put into place. Mrs Smith was diagnosed with nephrotic syndrome and supportive treatment was commenced. She was reviewed by either the renal team or myself until her AKI had resolved.
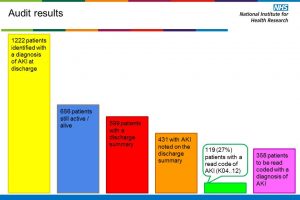
Within UHS we have an electronic system for discharge summaries. Our pathology electronic alert system for AKI is linked to our electronic discharge system to ensure that patients who have AKI have this included in the information given to primary care. I’m pleased to report that since her discharge Mrs Smith’s renal function has normalised completely.
Case studies