One of the most successful meetings of the last decade has been the Manchester Home Dialysis conference. Run under the stewardship of Sandip Mitra, for the last 9 years it has been the event to attend for patients, carers, industry and clinical teams with an interest in supporting dialysis at home.
And that support is needed. Despite the view that the UK underachieves in getting people onto home dialysis, be that peritoneal or haemodialysis, and the excellence of the meeting, progress remains slow. Low numbers at home and huge variation between centres remain at the heart of the issue. Why?
The why as it turns out is very difficult to nail down. Certainly, clinicians show a strong preference for home therapies when asked the question – especially if directed as a personal choice – as confirmed in BMC Nephrol. (2014 Jan 15;15:16. Nephrologists’ perspectives on dialysis treatment: results of an international survey. Fluck RJ, Fouque D, Lockridge RS Jr). Even a proportion of frail individuals might be suitable with the right support. Yet variation persists. The latest UK Renal Registry report has a range of home dialysis rates from 0-40% between centres in the UK. So what might be the real barriers?
At the 2016 conference, attendees and then the general nephrology community, responded to an online survey. Covering a broad range of expertise and clinical role, 185 individuals kindly completed the survey. The bar chart show the responses to one of the questions – patient factors in blue, resource factors in red and service factors in orange. A common discussion point is about finance, but in terms of barriers it was not felt to be the principle barrier. Patient factors were identified as a leading factor (in blue) followed by resources and service issues including staff knowledge. Business planning and resources were the biggest identified issues in those categories. What was interesting was that in centres with high leadership values organisational barriers and staff barrier ratings all fell significantly, from scores of 2.5 – 3.0 down to 2.0 – 2.2. This implies that good leadership is part of the solution to overcoming these problems. In contrast the perception of patient factors as barriers did not change. So, where there is a will there is a way! What can be done?
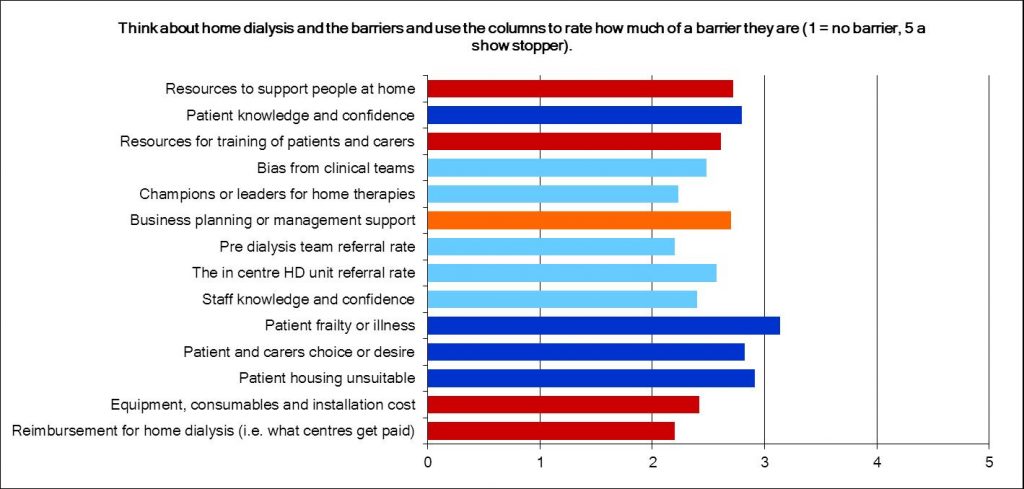
A realisation that the barriers are internal to the service – around leadership and knowledge – is quite useful. It tells us that the organisational system around commissioning and pricing is not the issue, it is how multiprofessional teams acquire the skills, knowledge and confidence to support people to undertake a home dialysis treatment. It is about the leadership and vision that gives the permission to change whilst providing some challenge to the way care is delivered. Simple words, simple ideas, not always easy to deliver. So, what is next?
KQuIP is committed to supporting a national programme of improvement for home dialysis. Working with networks of providers, a project structure will be developed by KQuIP, the UK Renal Registry, the Home Dialysis Conference experts and most importantly, you. Work is underway to design the project, find the funding and make a change. Be part of it and give us your thoughts. In the meantime: THINK HOME DIALYSIS!